Patient advocates have a collective understanding of the patient pathway, from the first suspicious symptoms to the realities of life as a survivor, that is unrivalled by any professionals. They also understand better than anyone how valuable that knowledge and experience is to people trying to navigate their way through a new cancer diagnosis. And they want to help.
That is one of the reasons why, seven years ago, the global network of GIST, Sarcoma and Desmoid patient groups (SPAEN) set about drawing up a patient pathway document that could offer newly diagnosed patients guidance that was easy to understand and could answer many of their questions about what should happen next.
“The aim was to give something that was very accessible to someone who had just been diagnosed and gave them, ideally in one page, a very clear picture of what the next few weeks or months were going to be like,” says SPAEN’s Roger Wilson, one of the document authors. “After the shock of diagnosis, and normally at primary treatment, most patients start looking at what’s happening to them and asking whether they’re getting the best.”
That was the how it started. But the plan took intensive research, consultation and time. When SPAEN published the final Sarcoma Patient Pathway in 2016, it was a seven-page document that mapped, as intended, what sarcoma patients should expect to happen along their diagnostic/treatment/ pathway. But it also included a parallel set of recommendations, aimed at healthcare systems, on developing quality sarcoma services provision.
The exact impact of the SPAEN document, acknowledges Wilson, is hard to measure. The fact that the document has been downloaded more than 4,000 times and hundreds of copies have been distributed offers some indication. Certainly many other European organisations have looked on with some awe at the SPAEN enterprise.
Yet its patient-targeted model has not been widely followed. One reason may come down to the sheer effort required to produce something sufficiently authoritative ‒ the SPAEN pathway was a mammoth effort, which had to take into account a vast range of clinical guidelines and variations in disease. For some in the patient advocacy world, the case still has to be made that the benefits of such a document justify the investment of time and money required.
“There is so much variation in countries and across Europe that it is really time consuming to gather and compile the information,” says Gilly Spurrier-Bernard, Vice-President of Melanoma Patients Network Europe (MPNE) and Chair of WECAN, the Workgroup of European Cancer Patient Advocacy Networks. “It’s difficult enough just getting clinical guidelines accessible and translated for eastern European languages.”
Variations within the cancer experience are another complication. The journeys of low-risk early-stagers and a high-risk metastatic population will be very different (SPAEN in the end had to include an additional pathway for advanced disease). “In melanoma, we now also have a relatively new moderate-risk adjuvant-treated population, who have a huge variety of pathways across Europe – with no access still in some countries in eastern Europe and elsewhere,” says Spurrier-Bernard.
Perhaps even more troublesome is the difficulty of producing anything that is both comprehensive and accessible to newly diagnosed patients, usable at every stage of their journey. The SPAEN guidelines, as they evolved through consultation with patients, professionals and international cancer bodies, and were brought into line with professional and clinical guidelines, subtly changed their nature and target group.
“[The] recommendations column in the pathway did creep in quite early,” says Roger Wilson. “I think it really came back from the patients, saying that they needed something to put on the table when making representations to medical directors or cancer centres that want to construct a sarcoma service. Decision makers need something to act on, to assess what a team needs to do to achieve an objective.”
While melanoma advocates have also worked on care pathways, the exercise is aimed at providers as a means of leveraging better services
So the SPAEN pathway, which started as a compass aimed at patients, became more a set of patient-facing guidelines aimed at professionals. The latter, says Gilly Spurrier-Bernard, is perhaps the more practicable route, and is the one that MPNE has followed. So while MPNE has also worked on care pathways, the exercise is aimed at providers as a means of leveraging better services. They focus on identifying ‘pain point’ blockages, and are specific to particular countries and situations.
“It is useful to us when we need to map a particular issue,” she says. “But variations in Europe can make it a huge exercise. Even aligning with the European Cancer Organisation’s Essential Requirements for Quality Cancer Care has been tricky.”
The variations also mean that patients are unlikely to be able to identify with any ‘average’ pathway aiming to help them orientate themselves. “They have to be able to see themselves on the pathway for the document to be helpful, and because of variations in hospital, mutation, imaging and so on, most individuals don’t see themselves as the ones being referred to.”
And there’s another worry. Yes, it is good that clinicians and industry want to support and be involved in initiatives that are based around giving patients a sense of where they are and what should happen next if they are getting the best treatment. But she feels that, when clinicians take the lead, it can be hard to avoid pathway documents reflecting their own assumptions about what matters and what is ‘best’.
“There’s a danger that these things aren’t used much, because what the clinicians propose is based on what they think patients need, and their own unresolved confusions about this creep in. That means that things are far from simple when it comes to clearly and diagrammatically explaining ‘what comes next’.”
Richard Price, EU Affairs Policy Manager at the European Cancer Organisation recognises that there is a challenge here. Amid all the guidelines and pathways for optimal care that are produced in the world of cancer, and for all the efforts to include a patient perspective, there is always the risk that the clinician view of care dominates.
Since 2017, the European Cancer Organisation has published Essential Requirements for Quality Cancer Care (ERQCCs) – checklists and explanations of the organisation and actions needed to achieve high quality cancer care. They are, in effect, organisational specifications – ‘roadmaps’ as Price describes them – designed for a wide readership including oncology teams, patient advocates, policymakers and managers.
Price says they tap into a wider picture of European initiatives such as the European Union’s Innovative Partnership for Action Against Cancer (iPAAC), where patient representation is vital. But the fact is that much guidance has not always been sufficiently patient-focused.
“Efforts need to increase to ensure cancer patients are empowered with the right information following a diagnosis and throughout their journey through treatment and follow-up. Yet, beyond this, we should also be helping cancer patients to achieve a stronger sense of their rights as a patient,” says Price. Recognising the need for something less technical, the European Cancer Organisation came up with an accessible European Code of Cancer Practice, setting out a general set of core requirements for good clinical cancer practice, which was co-produced by a team of cancer patients, patient advocates and cancer professionals.
“What we feel is important is to have patients helping to drive the creation process right from the very outset. If patients aren’t in the first meeting and key decision-making roles something doesn’t feel right. It’s much harder, perhaps impossible, to make something patient-centred and patient-focused by patient involvement later on.”
For patients or for service providers?
The ingredients for a useful pathway document, then, seem to be twofold. First, you need clarity about whose perspective it represents: patient, clinician or policy maker? Ticking a patient input box doesn’t mean this is a patient perspective.
Second, you need to be clear who the document is aimed at. The tone, detail and priorities of an orientating pathway aimed at a newly diagnosed patient will be very different from a standard-setting pathway of requirements aimed at care providers.
New European patient-led initiatives in colorectal cancer have had these guiding principles in mind. One of those steering and compiling them has been Stefan Gijssels, Co-Founder of Digestive Cancers Europe, the European umbrella organisation representing patients with colorectal, gastric and pancreatic cancers.
“Patient pathway documents targeted at service providers, that also offer patient-focused recommendations for improvements, is the way to go”
He believes that producing patient pathway documents targeted at providers, that also offer patient-focused recommendations for service improvement, is definitely the way advocacy groups should be heading.
Offering patients the orientation and support material they need to help navigate their journey remains a key role for advocacy groups, he stresses. But what they want and need to know at a very stressful time is not the same as what service providers need to know to better meet the needs of patients. As Gijssels stresses, the onus should not be on patients having to know what processes should be happening when: it’s the decision makers who should be building effective pathways into their systems.
To help patients identify the topics that need to be addressed during the treatment period and address their support and information needs, Digestive Cancers Europe is currently producing what it calls a ‘Patient Navigator’ . This is a booklet and app that will be made available via oncologists, providing simple information about what to consider at each stage after diagnosis: treatment options, questions to ask your doctor, trusted sources of information, the sorts of conversations you may need to have with family, signposts on nutrition, physical activity, work and finance.
This is totally by and for patients. There is no need for the completeness that clinicians and policy makers need to precisely define the pathways involved in such a complex area of medical practice. “That’s the last thing a patient needs. I think we have to start with clarity ‒ and then once you want to know more, then you can dig to a level deeper and we provide the information in more substance.”
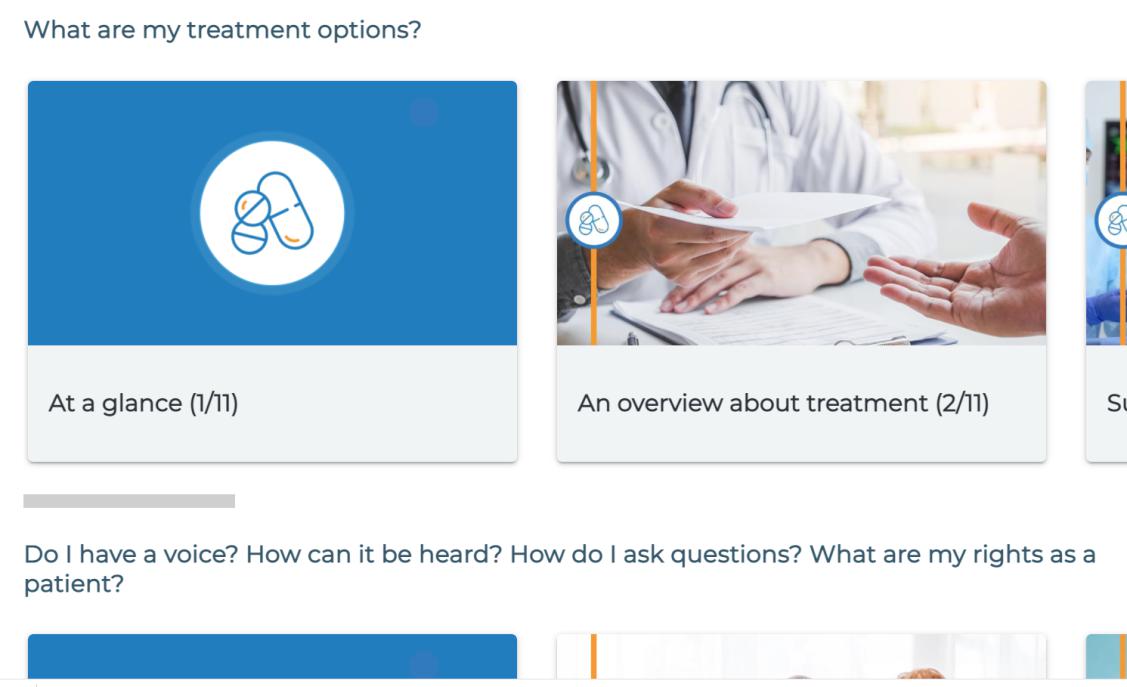
Source: Screenshot of https://digestivecancers.eu/gpscrc/ 27 February 2021
As a separate exercise, Digestive Cancers Europe is working on two pathway guidelines aimed at managers and clinicians. They are fundamentally different than most of the clinician-led guidelines and pathways produced by many cancer organisations across Europe. They turn their model on its head.
“We’ve integrated shared decision making throughout, with… patients engaging with patient organisations prior to any treatment decisions”
The first pathway, due to be published in 2021, is being developed as part of the iPAAC project work package on Governance of Integrated and Comprehensive Cancer Care. It is a patient-focused linear pathway of ‘process’, specifying all the steps that need to be taken by a hospital, in consultation with the patient, from diagnosis of colorectal cancer to discharge (a similar pathway is also being developed for pancreatic cancer). “We’ve integrated elements of shared decision making throughout, with patient consultation and patients engaging with patient organisations prior to any treatment decisions,” says Gijssels. It is currently being piloted at the Charité Hospital in Berlin.
“It’s critical that the right sequence is followed, and that you are treated by the right experts in the team. But from a patient perspective, it’s very important that you can put your finger on the pause button. Very often, a treatment plan is decided at the same consultation where the diagnosis has been given. But it’s such an emotional moment you don’t hear anything. And you are sucked into a system that you do not control.”
“So from a patient perspective it’s very important to be able to inform yourself and have the possibility of taking a step back and saying: okay, what does that now actually mean? This needs to be built into systems. Maybe have conversations with peers who have gone through the same thing, gather more information, think about questions to ask.”
The other guideline initiative from Digestive Cancers Europe is the European Colorectal Cancer Roadmap, due to be published in 2021. This goes through every step of the patient journey, from screening through to end of life, and uses the most recent data to evaluate – from a patient perspective – just how well services are doing in key areas. It then provides recommendations on how some countries can improve and apply the best practice that is succeeding elsewhere.

It is providing some shocking findings, with mortality rates one month after colorectal cancer surgery 14 times higher in some hospitals than in others. The point is, says Gijssels, that the Roadmap will provide analysis and recommendations for a way forward from a patient perspective – something for policy makers to get their teeth into that genuinely matters in terms of the experience of services, not the administration of them. It includes patient-centred recommendations on surgery, radiotherapy, oncology treatment, drug availability and psychosocial care.
This should be the real role of patient advocacy groups in producing pathways, says Gijssels. He knows from personal experience that patients find it hard to take in information at the time of diagnosis and afterwards. Tools to help patients orientate themselves have a use, but it’s policy makers and clinicians who should be the main target of pathways.
“I think we want to force policymakers and make medical practitioners to think in a more holistic way,” he says. “Everybody looks at care in a very fragmented way from the perspective of their own systems or technology. But there is no bird’s eye view of what really needs to happen to make our healthcare system more sustainable and rational.”
“It’s bizarre from a patient perspective, for example, that it can take so long to get a correct diagnosis”
“It’s bizarre from a patient perspective, for example, that it can take so long to get a correct diagnosis. I had surgery twice because the first time they completely underestimated the severity of the metastasis. Another example is that I have problems in both my colon and my stomach – but it’s impossible to have a colonoscopy and gastroscopy on the same day, because apparently it’s too difficult to organise.”
“Everybody talks about efficiency of the healthcare system but not from a patient perspective. That means that often they are missing the obvious things.”
Roger Wilson agrees. Five years on, the SPAEN pathway is now in need of review, given advances in understanding and technologies. The next version could look very different, says Wilson. “But what we must not lose is the principle that it is led by patients who make it relevant for other patients.”
The real lesson of the last decade’s experimentation may be that patient pathways’ greatest value is not in assimilating huge amounts of complex knowledge, but in making the urgent simplicity of patients’ needs strikingly and unavoidably obvious.