Reports of the results of two antibody-drug conjugates (ADCs), one for HER-low metastatic breast cancer, the other for metastatic lung cancer resistant to EGFR inhibitors, highlight the advances being made in this type of treatment. The DESTINY-Breast04 study, presented at ASCO 2022 , and published simultaneously in The New England Journal of Medicine, June 5, found that, compared to conventional chemotherapy, trastuzumab deruxtecan (T-DXd) reduced risk of disease progression by 50% and death by 36%.
“The strong efficacy of T-DXd in this HER2-low patient population supports the need to now reclassify HER2-low as a new therapeutically targetable category of metastatic breast cancer,” said lead investigator Shanu Modi, a medical oncologist at Memorial Sloan Kettering Cancer Center, New York.
Among breast cancer patients without HER2 amplification, overexpression, or both, a large proportion express low levels of HER2. Traditionally, patients with low levels have been grouped with HER2 negative patients, limiting their possibilities for treatment with trastuzumab.
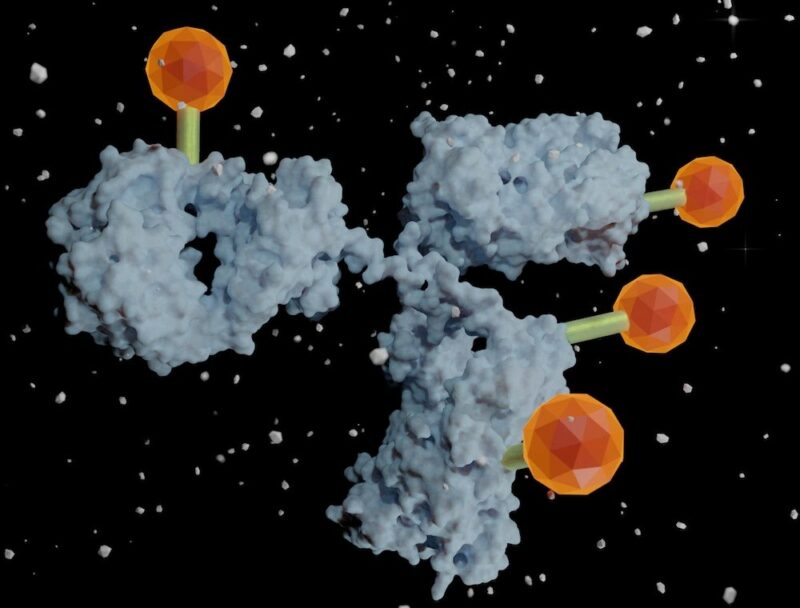
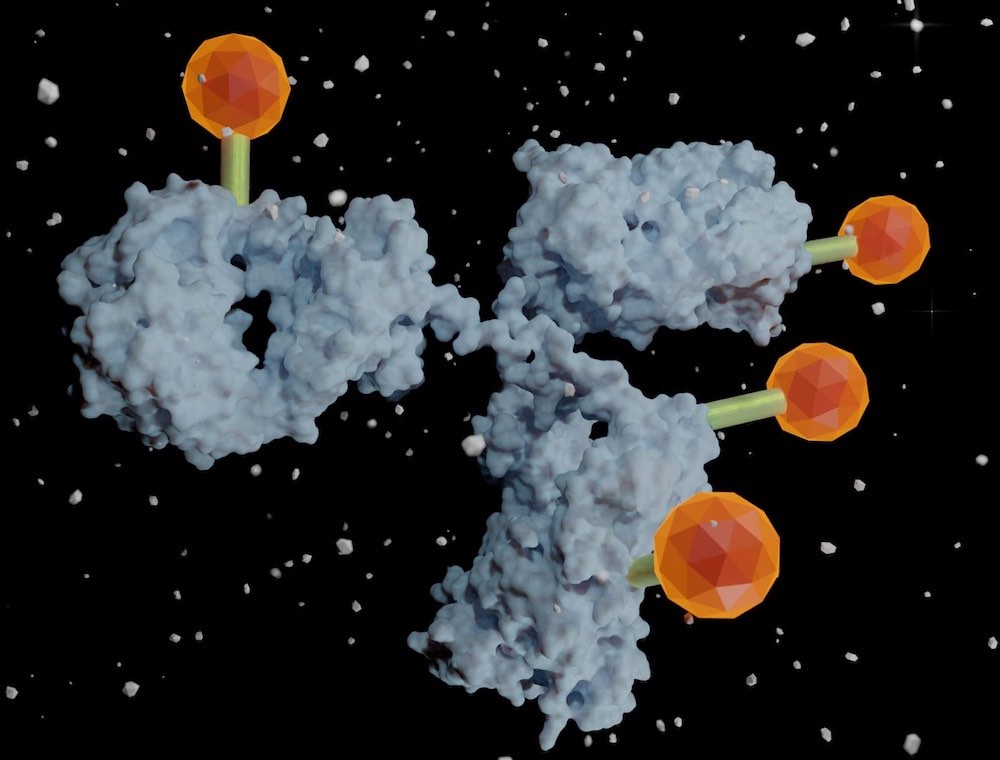
T-DXd is an antibody-drug conjugate consisting of a humanised anti-HER2 monoclonal antibody linked to a topoisomerase I inhibitor payload that interrupts DNA replication in cancer cells. In May 2022, T-DXd was approved by the FDA for use in adults with unresectable or metastatic HER2-positive breast cancer who have received prior anti-HER2-based regimens. However, unlike many other approved HER2-targeted therapies T-DXd can also target tumour cells expressing low levels of HER2, by using HER2 to serve as a ‘homing beacon’ for the delivery of highly cytotoxic chemotherapy. After T-DXd binds to HER2 and becomes internalised, the payload is liberated, killing the targeted tumour cells by causing DNA damage.
The current DESTINY-Breast04 study set out to evaluate the efficacy and safety of T-DXd in patients with HER2-low metastatic breast cancer. In the phase III study, 577 patients with HER2-low metastatic breast cancer, who had been treated with one or two prior lines of chemotherapy for metastatic disease, were randomised 2:1 to receive either T-DXd (n= 373) or the physician’s choice of standard chemotherapy (n= 184, capecitabine, eribulin, gemcitabine, paclitaxel, or nab-paclitaxel). T-DXd was administered intravenously every three weeks at a dose of 5.4 mg per kilogram of body weight. A key consideration for the study was the ability to identify cancers with HER2-low status.
Of 557 patients who underwent randomisation, 494 (88.7%) had hormone receptor-positive disease, and 63 (11.3%) had hormone receptor-negative disease.
For the hormone receptor-positive group, median progression-free survival was 10.1 months for the T-DXd group versus 5.4 months in the physician’s choice group (HR=0.51, P<0.001), and overall survival was 23.9 months for the T-DXd group versus 17.5 months for the physician’s choice group (HR=0.64; P=0.003).
Among all patients (hormone receptor positive and negative), median progression-free survival was 9.9 months for the T-DXd group versus 5.1 months for the physician’s choice group (HR=0.50; P<0.001), and overall survival was 23.4 months for T-DXd group versus 16.8 months for the physician’s choice group (HR=0.64, P=0.001).
The overall safety profiles of T-DXd and chemotherapy were similar with respect to grade 3 or higher treatment emergent adverse events (TEAEs 53% T-DXd vs 67% chemotherapy, serious TEAEs 28% vs 25%, and TEAEs associated with death 4% vs 3%). In the T-DXd group the most common grade 3 or higher adverse events were neutropenia (13.7%), anaemia (8.1%), fatigue (7.5%), leukopenia (6.5%), thrombocytopenia (5.1%), and nausea (4.6%). Interstitial lung disease, an adverse event of special interest with T-DXd, occurred in 12.1% of patients, developing at a median of 129 days (range 26–710).
Discussant Patricia LoRousso, from Yale University, said, “Should standards of care for patients with HER2-low breast cancer change as a result of the data Dr Modi presented today from DESTINY-Breast04? My answer to you is ‘absolutely’.”
LoRousso added that more sensitive and objective assays of HER2 status will be needed to identify patients with low levels of HER2 expression who may be suitable for T-DXd treatment.
Dr Modi said that two studies are currently ongoing to determine the minimum HER2 expression threshold for T-DXd activity, adding that T-DXd may also be effective for patients with HER2-mutated disease, for whom there are currently no treatments.
T-DXd is currently under review for the treatment of adults with unresectable or metastatic non-small-cell lung cancer whose tumours have a HER2 mutation and who have received a prior systemic therapy.
In a second abstract presented at ASCO, the ADC patritumab deruxtecan (HER3-DXd) showed significant clinical activity in non-small-cell lung cancer (NSCLC) resistant to treatment with EGFR inhibitors. It is estimated that about 83% of all NSCLC tumours express the HER3 protein, which is associated with increased incidence of metastases, reduced survival, and resistance to standard of care treatment.
In the phase I dose-escalation/ expansion trial, 57 patients with locally advanced/ metastatic EGFR-mutated NSCLC and disease progression on prior EGFR TKI treatment received HER3-DXd.
Results showed that HER3-DXd led to objective responses in 22 of 57 patients, and to stable disease in 19 others. The disease control rate (response plus stable disease) was 72%. An analysis of antitumour activity in 25 patients with brain metastasis showed objective responses occurred in eight patients and stable disease in 12 patients, giving a disease control rate of 80% for this group.
“The striking finding of this study is reported activity of patritumab deruxtecan across all reported resistance mechanisms including EGFR-related and non-EGFR/ MET related,” said study presenter Pasi Jänne, from the Dana Farber Cancer Institute, Boston.
Commenting on the studies Giuseppe Curigliano, from the European Institute of Oncology, Milan, said, “Multiple histology-agnostic therapies are currently adopted in clinical practice for treating patients regardless of their tumour site of origin. In parallel with this new model for drug development, in the past few years, several novel antibody–drug conjugates (ADCs) have been approved to treat solid tumours, benefiting from engineering improvements in the conjugation process and the introduction of novel linkers and payloads. With the recognition that numerous surface targets are expressed across various cancer histologies, alongside the remarkable activity of modern ADCs, this drug class has been increasingly evaluated as suitable for a histology-agnostic expansion of indication. The anti-HER2 ADC trastuzumab deruxtecan has demonstrated compelling activity in HER2-overexpressing breast, gastric, colorectal, and lung cancer. Examples of additional novel and potentially histology-agnostic ADC targets include trophoblast cell-surface antigen 2 (Trop-2) and nectin-4, among others.“