A decade ago, men with metastatic prostate cancer could typically expect to live two to three years. The arrival of new hormone drugs such as abiraterone radically changed the odds, and the equation is now changing every day, as trials investigate new biomarkers and drug targets, with a growing number of precision medicines, such as PARP inhibitors, now becoming available for men with the relevant genetic profile.
The good news is that prostate cancer care has entered the world of precision medicine. The bad news is that many cancer services have not. Too often they are built around a one-size-fits-all approach, which means patients are missing out on precision treatments that could extend their life and quality of life, expensive drugs are being wasted on people they’re not suited to and trials are going undersubscribed.
The question of how to get the precision treatments into the precise group of people who can be expected to benefit is one of the big challenges of oncology today. An innovative Berlin-based project is piloting a possible solution, focused initially on people with advanced prostate cancer living in the region. Since its official launch in February 2020 the initiative has drawn widespread praise from patients and clinicians alike.
No one left behind
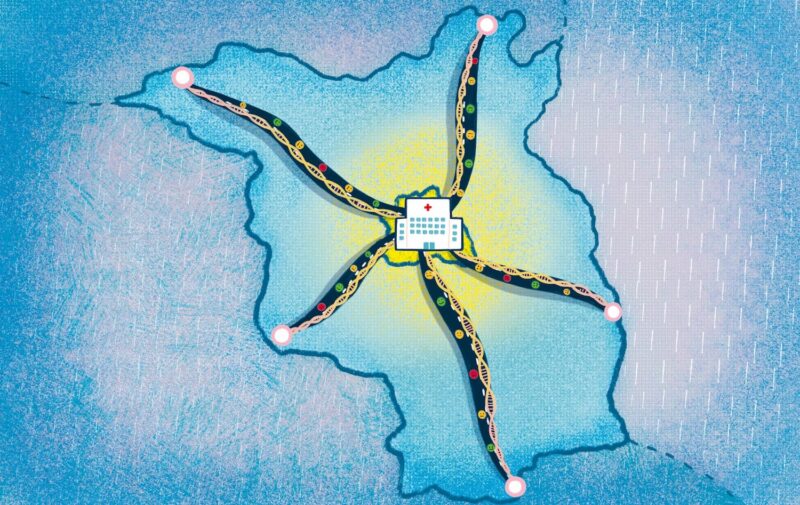
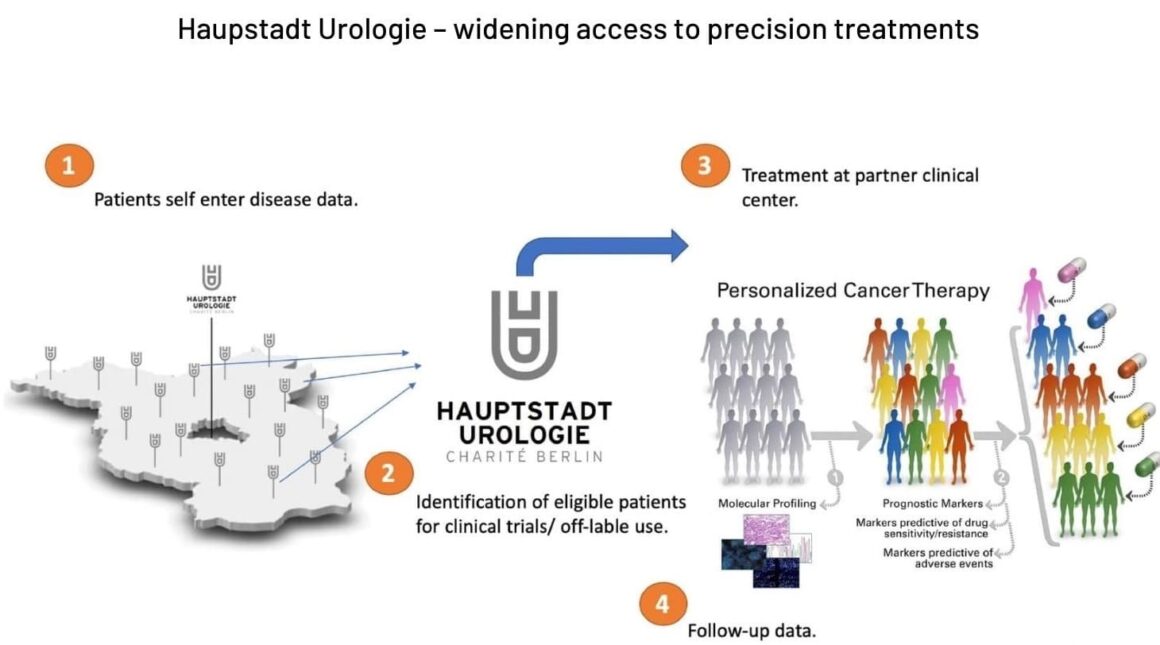
The Hauptstadt Urologie (Capital Urology) project was started at the Charité Universitätsmedizin in Berlin, one of Europe’s largest university hospitals, serving four million people. It seeks to make the hospital’s plentiful expertise and technology available beyond its immediate catchment area – to the three million people living in the surrounding state of Brandenburg, an area of 30,000 square kilometres.
The project aims to use a personalised approach throughout the patient journey, from diagnosis to relapse management and end of life. And it all revolves around an electronic network connecting men with prostate cancer and local urologists up to the expert staff and resources at Charité. The lifeblood flowing through the network is data.
“The idea is to serve those in the periphery who are normally all too easily disconnected from medical progress”
The idea, says Thorsten Schlomm, who jointly created the project with health systems analyst Tim Rödiger and his team, is to serve those in the periphery who are normally all too easily disconnected from medical progress. The project involves more than half of the 240 treating urologists in Brandenburg, each the centre of a micronetwork of around 3,000 patients, with every patient able to individually input data about themselves into a centralised system via a home computer or a mobile phone app.
One database for treating and learning
“What we do is get all the relevant disease-specific data out of the brains of the patients, into our database,” says Schlomm, who is Professor of Urology and Director of Urological Clinics at Charité. “Normally you have data silos, with different bits of data in different places, and it’s impossible to get all these bits of data back in one system. We have developed a system to centralise and structure all this data.”
The beauty of including self-reported patient data in this mix is that patient reported outcomes (PROs) become intrinsic to the system. Patients record, side effects, pain and quality of life. Combining this with their molecular and medical data, patterns begin to emerge.
“With the data, we can group patients according to biological and therapeutic events and, with a ‘nearest neighbour’ algorithm, sort patients so that we can identify those with similar disease,” says Schlomm. This allows clinicians and researchers to look at why patients with similar disease may experience a different disease course and quality of life. “We start to see patterns, and this allows us to recommend a best therapy and identify patients of interest for drug trials and molecular therapy studies.”
Patients are recruited via the local urologists, who continue to be their main point of contact. More than 300 men with castration-resistant advanced prostate cancer are already on the database, with new entrants joining every month. Recommendations for treatment, off-label prescription and clinical trials come from the Charité experts, but patients – who may live more than 100 km from Berlin – do not have to travel there.
Source: Courtesy of Thorsten Schlomm, Haupstadt Urologie
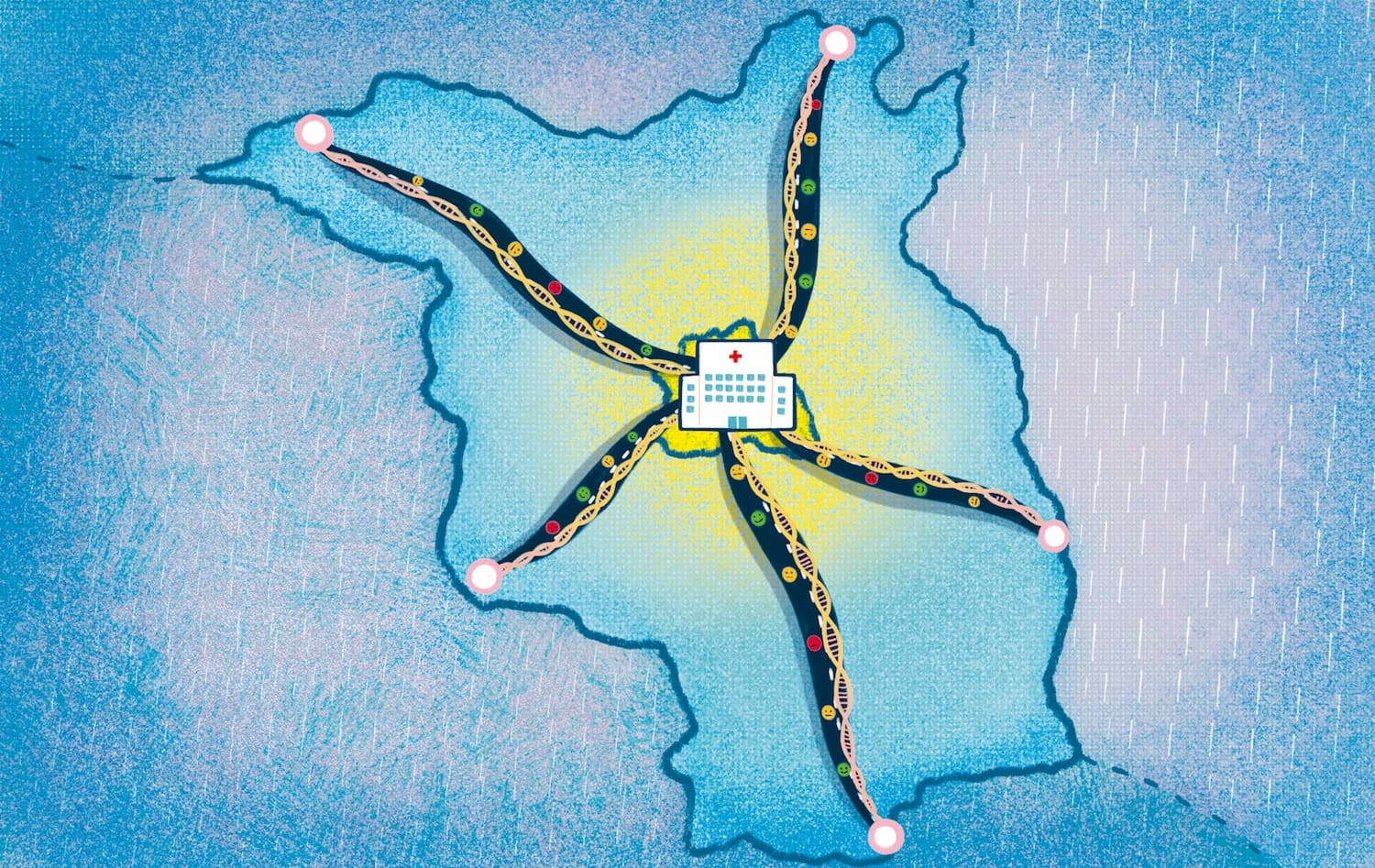
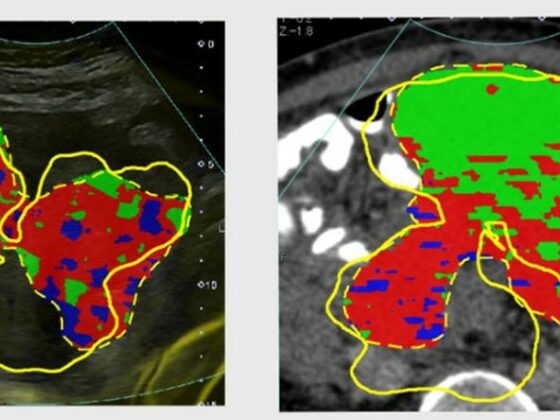
Around 50‒60% of advanced prostate cancer patients in Hauptstadt Urologie are invited for tumour genome sequencing. The genetic tumour assessment gives patients the option of a precision treatment – selected by applying algorithms to their personal data. Those with a BRCA or other mutation affecting DNA repair receive a PARP inhibitor (olaparib was approved for use in advanced prostate cancer in the EU in November 2020). Some patients are invited to enter ‘basket trials’ of new drugs; for example, patients with PTEN deletions qualify for trials of new AKT inhibitor drugs.
“Patients are happy because they get the best care and outcomes. Health insurers are happy because money is not being wasted on unsuccessful treatments”
According to Schlomm and Rödiger, everyone benefits. Patients are happy because they get the best care and outcomes. Health insurers are happy because money is not being wasted on unsuccessful treatments. And drug companies are happy because their drugs are being used and trials are well subscribed.
“A clinical trial is very expensive and if you are able to close the trial one year earlier you can bring a drug to market earlier, help patients earlier and increase revenue,” says Rödiger, Principal and Partner at Die BrückenKöpfe, a German healthcare thinktank. “Patients, doctors, oncologists, regulators, insurance all like it because it provides such a clear and transparent structure.”
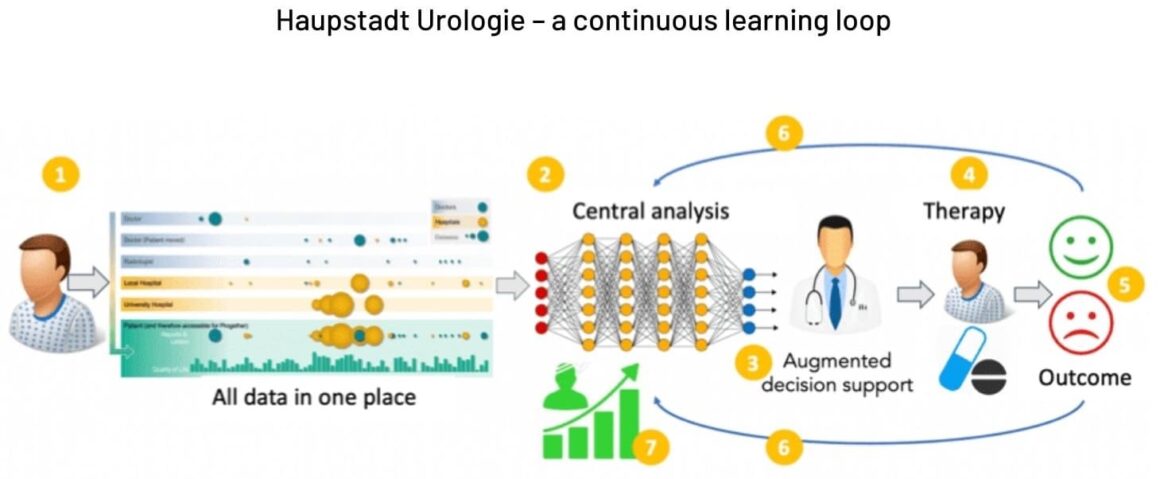
2. Data are continuously screened for optimal therapy options
3. Recommendations are forwarded to the treating doctor in the perip[hery (augmented decision support)
4. The patient is treated
5. Outcomes (treatment response, side effects and quality of life) are continuously updated and recorded
6. Outcome data are continuously fed I, and improve the algorithms (feedback loop)
7. The process continuously increases real-world data resources for research and improvements
Source: Courtesy of Thorsten Schlomm, Haupstadt Urologie
A model for other cancers?
The pilot has already caught the eye of patient organisations internationally. “It’s an interesting project, tackling the persistent problem of getting top-notch care to cancer patients in the periphery,” says Bettina Ryll, founder of Melanoma Patient Network Europe. “It supports local oncologists with diagnostics and expertise, so patients can receive highly specialised care close to home. It is set up in collaboration with payers and integrates research into routine clinical care. From an advocate’s perspective, I’m obviously interested to see how patients can access and use their own data, and how the overall dataset is used to drive research. As a cancer patient, you want as many smart brains working on your problems as possible.”
“As a cancer patient, you want as many smart brains working on your problems as possible”
Healthcare professionals are interested too. Silke Gillessen, Senior Consultant in the Department of Oncology and Haematology at the Kantonsspital St. Gallen in Switzerland, and a specialist in advanced prostate cancer, likes the early signs. “It is a very good approach, in my eyes, to bring urologists into the university network and to propose therapy studies if a patient seems eligible.”
Whether the Hauptstadt Urologie approach can be easily replicated elsewhere is another question. It arose in a country with a very specific multi-payer and locality-based healthcare system, where urology diagnosis, treatment and follow-up are handled separately – often by different doctors. It was also the product of a the unique coming together of people and funding.
Until 2018, Schlomm was Senior Physician and Scientific Director at the Martini-Klinik, University Hospital Hamburg-Eppendorf – a German prostate cancer centre of excellence, combining public and private treatment and renowned for its molecular research. While there, he established the Progether network – a tool to connect patients and enable them to learn from the experience of others. This network was seed-funded by former prostate cancer patients and developed with researchers from the Fraunhofer Institute in Darmstadt, led by Sebastian Maier.
When Schlomm was appointed Professor of Urology and Clinic Director of the Urological Clinics at Charité in 2018, he decided to take this project to the next level, integrating genomic data with information from large numbers of patients and clinicians over a wide area, and creating a single system for decision-making and providing the highest quality treatment possible. The German Human Genome and Phenome Archive was to manage the genomics data. With such collaborators, and Schlomm’s track record, the initiative was supported by the Ministry of Health, insurers, regulators and the pharmaceutical industry.
The start-up funding for the five-year Hauptstadt Urologie project comes from private donations and partnerships with main players, income from advisory services to companies interested in precision medicine, and an operating-cost loan. This is now being supplemented by income from real world studies, contracts with health insurance companies and digital health apps.
“We are already working on extending it to bladder cancer, the next biggest cancer in urology”
With the advanced prostate cancer pilot now proving its worth, Schlomm and Rödiger are now looking to expand the Hauptstadt Urologie approach to other cancers and regions within Germany.
“We are already working on extending it to bladder cancer, the next biggest cancer in urology, and melanoma, because we have a good group of melanoma specialists at Charité,” says Schlomm. “Then ovarian cancer and endometrial cancers. All have significant molecular alterations which are routes to molecular therapies, and the tumours with the greatest medical need for precision diagnostics.”
Rödiger says other organisations and institutions in Germany are now approaching them. “They are saying ‘We need this,’” he says. And he is in conversation with the Government about regulatory changes that might be needed if the scheme were to become more widespread. “But we don’t need the Government to say that everyone now has to start doing network medicine like Hauptstadt Urologie,” he says. “If people like it and want it that’s okay, but we don’t want anyone to say you have to do it this way.”
Sustainability is a challenge
Rödiger says the project has a firm financial base for the next five years. But some of the financial realities of expanding the project, and making it long-term, are becoming plain.
“There is a resource problem making precision medicine accessible for everyone,” he says. “We don’t have the resources to carry on doing things the way we do them now, so we are now automating and optimising a lot of our processes. First we have to automate, and then we can roll out next year to other regions and indications.”
“There is a resource problem making precision medicine accessible for everyone… so we are now automating and optimising a lot of our processes”
Günther Carl, a German patient advocate and Vice Chairman of Europa Uomo, the European Prostate Cancer patient coalition, has witnessed the project’s gestation and birth. He is impressed. But he also has worries about long-term funding.
“I know six patients who are under the umbrella of the scheme, and there’s no doubt it’s the very best you can do at the moment.” Local urologists, he says, have a large throughput of patients and it’s impossible to keep on top of the recent science, so giving them access to such a source of expertise is badly needed. “With Hauptstadt Urologie they get a detailed recipe of what to do, based on state-of-the-art science. It’s a brilliant idea. I only hope they have the money to make it sustainable.”
Carl believes the project has much in common with work at the Martini-Klinik, but that organisation has private funding and its network extends only to the Hamburg area. Hauptstadt Urologie has much greater ambitions.
“I think the aim of Charité is to extend its reach through old Eastern Germany,” he says. “I think it will certainly be a formula that some other big university hospitals can follow. But funding is usually a bottleneck in all university clinics, so it will be interesting to see if they can overcome this, as Schlomm did with his backing and connections.
“If the project has success it can be copied. I know there are professors in Europe who would like to progress in a similar way. The point is that in Europe, as with Germany, you have to evaluate city by city, university by university, to see if there is sufficient funding flow to have the luxury of creating such high-level, patient-centred medicine.”
Over the next five years, the world of cancer – not just those with an interest in advanced prostate cancer – will be watching.
Illustration by: Sara Corsi