Going back to the nineteenth century there were reports that infectious diseases seemed to provide brief periods of remission for cancer patients. One case from 1896 reported that the enlarged spleen of a woman with “myelogenous leukemia” shrank to nearly normal size when she contracted influenza (Dock G, Am J Med Sci, 1904). “It wasn’t until a little later on when viruses were actually discovered, that correlations began to be made,” says Adel Samson, who leads the Translational Cancer Immunotherapy Group at the University of Leeds. From the 1950s onwards serious attempts were made to therapeutically harness the effect of ‘oncolytic viruses’ − viruses that cause cancer cells to disintegrate − but only in the past two decades have significant advances been made and a wave of oncolytic viral therapies is now entering the cancer treatment landscape.
The first oncolytic virus to be approved by a national regulatory agency was RIGVIR, a non-pathogenic enterovirus, approved in Latvia in 2004 for the treatment of melanoma, but withdrawn in 2019 due to a lack of data supporting its efficacy. In 2006 the H101 oncolytic adenovirus was approved in China for the treatment of head and neck cancer. The first approval in Europe and the USA came in 2015, with talimogene laherparepvec (T-Vec or Imlygic, from Amgen), a modified herpes simplex virus (HSV) approved for subsets of patients with melanoma. When injected directly into lesions it generates an immune response against the patient’s cancer. Real world data has shown response rates of up to 88.5%, with complete response rates of up to 61.5% (Franke V et al. Int J Cancer, 2019).
Given that the effects of viruses have been known for over a century, progress in exploiting their therapeutic value seems to have been slow. “One reason is that people came from different [disciplines],” says Angelica Loskog, from Uppsala University, Sweden, and CEO at Lokon Pharma. Research started in virology, but it has been the recognition of the importance of cancer immunology and the ability to genetically engineer viruses that has allowed the field to flourish, according to Gabriella Campadelli-Fiume, a virologist from the University of Bologna, Italy, whose lab has developed their own oncolytic HSV strain. Following approval of T-Vec by the US and European regulators, research “literally exploded,” she says. There are currently almost 40 clinical trials of oncolytic viruses recruiting patients, covering a variety of cancer types.
Harnessing the immune system
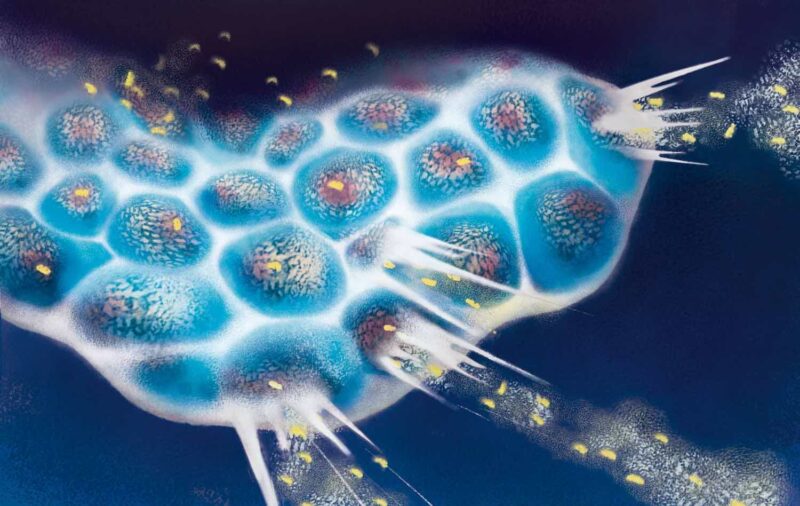
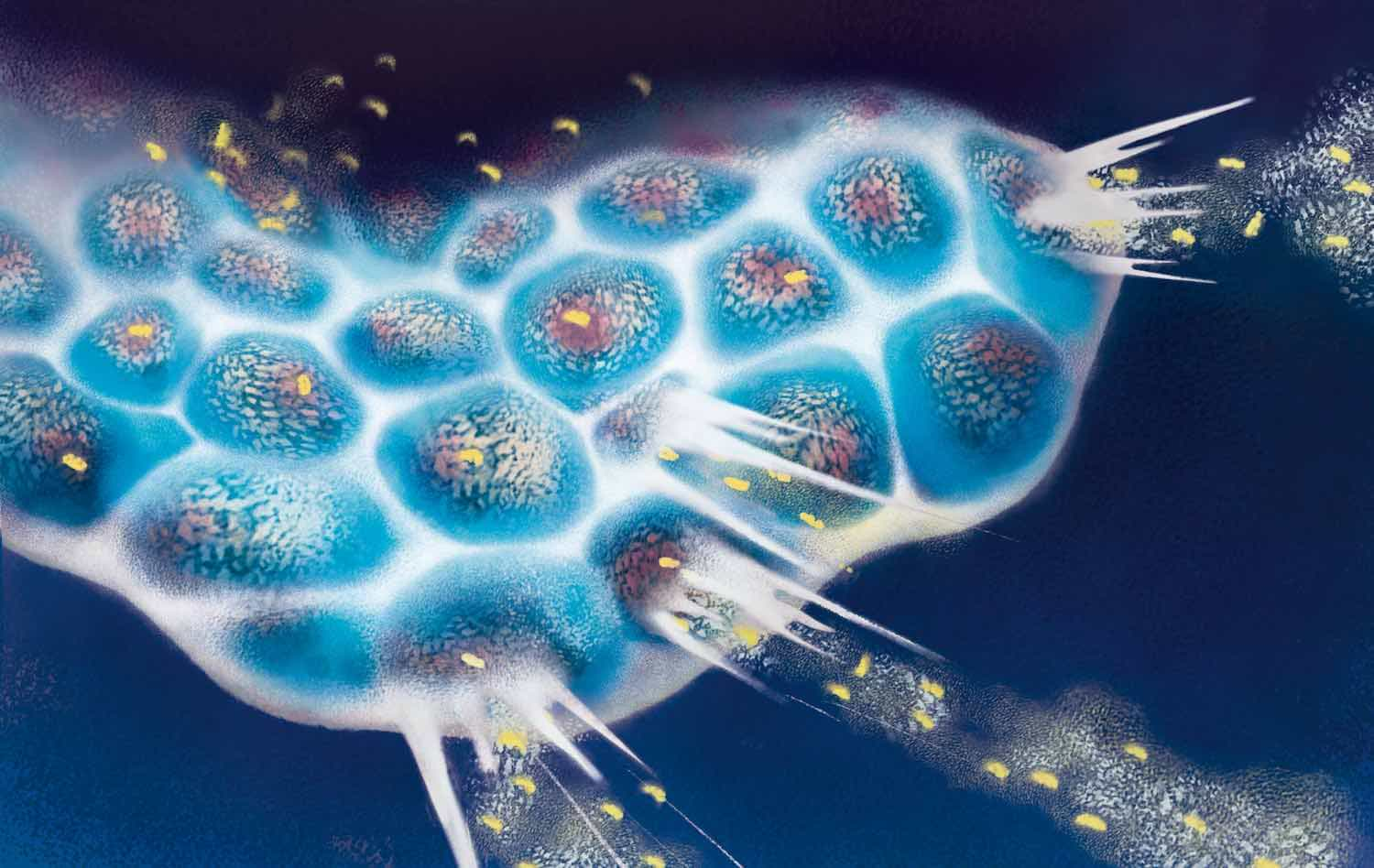
Why some viruses are able to preferentially infect and kill cancer cells is only partially understood but seems to be connected to the changed metabolic status of cancer cells that makes viral replication favourable. The viral infection will then cause tumour cell lysis − the cells disintegrate. But it has become clear that the real power of oncolytic viruses is their ability to harness the immune system into further attacking cancer cells. “There’s really a kind of natural synergy between the antiviral response and anti-tumour response,” explains Eric Quéméneur, chief scientific officer at Transgene, a clinical stage biotechnology company developing oncolytic viruses, based near Strasbourg, France.
Once lysis occurs, cancer cells release signalling molecules that are able to utilize the body’s immune system. The released signals, which include a cascade of chemokines and interferons ultimately induce immunogenic tumour cell death and subsequently restore the ability of dendritic cells to prime antitumour T cells.
A number of viruses including adenovirus, reovirus, measles, herpes simplex, Newcastle disease virus, and vaccinia have been clinically tested as oncolytic agents. Although some, such as reovirus and the senecavirus, occur naturally, most will be genetically engineered so they cannot damage healthy cells. “You have to manipulate the genome so they will be selective, and [for our] adenoviruses we decided to remove one gene that otherwise stimulates the virus replication… so it can only replicate if it is in a tumour cell,” explains Loskog. Transgene are using the vaccinia virus, which has proved safe for many years. ‘The strain we’re using now are double deleted in the sense that two genes have been destroyed, to improve the selectivity for replication in the tumour cells compared to normal cells,” says Quéméneur.
“The approach taken by my laboratory has been quite different,” says Campadelli-Fiume. “We modified the ‘key’ that HSV uses to enter and infect cells.” By modifying a surface glycoprotein, the virus becomes ‘retargeted’ and infects only cancer cells with the corresponding tumour-associated antigens on their surfaces. “The retargeted oncolytic HSVs are not attenuated, hence they are very effective at killing the cancer cells, and at eliciting anti-tumour immunity.” This will make these viruses specific to cancers carrying this antigen across indications ‒ the HER2 antigen, for example, is present in a fraction of glioblastomas, breast, stomach, lung, and pancreas cancers. Campadelli-Fiume has also generated viruses retargeted to some prostate cancers and brain tumours.
Modifying the immune response
“We were a bit naive on the type of response we could generate with the first-generation viruses,” says Quéméneur. Early work indicated it was not enough to rely on the virus’s innate ability to kill cancer cells, because the body’s own anti-viral defences are able to shut them down. “People now realise that the immunological part of oncolytic viruses is what is important,” says Loskog. “It’s not so much about the oncolysis, but more about what kind of transgenes we put into the viruses to make the tumour microenvironment really stimulatory.” Quéméneur says the current third generation of oncolytic viruses are engineered to improve the immune response by producing immune stimulatory agents. “We call them payloads,” he says. “Those additional genes that we put in the virus would be delivered specifically in the tumour… we could add antibodies, enzymes, or whatever function would be beneficial in changing the phenotype of the tumour.”
“It’s not so much about the oncolysis, but more about what kind of transgenes we put into the viruses to make the tumour microenvironment really stimulatory.”
The approved oncolytic virus T-Vec has been modified to express granulocyte-macrophage colony-stimulating factor (GM-CSF) − a cytokine that stimulates the movement of cells towards sites of inflammation or infection to mount a co-ordinated immune response. Another oncolytic virus being developed by Transgene, BT001, has included a second genetic modification, that also encodes for an anti-CTLA-4 antibody. The antibody is able to deplete the levels of regulatory T cells (also called Tregs), which are known to suppress other cells in the immune system. The BT001 virus has shown cure rates of 70% in multiple mouse models (Semmrich M et al. J Immunother Cancer, 2020).
Transgene has also developed an oncolytic virus, TG6002, which expresses an enzyme able to convert the molecule 5-fluorocytosine (5-FC) into the chemotherapy agent fluorouracil (5-FU). When the pro-drug is administered to the patient orally, the enzyme will be present only in cancer cells, allowing high concentrations of the drug to be produced within the tumour, whilst limiting chemotherapy-induced side-effects in other tissues (Abstracts, Human Gene Therapy, 2014). The company has announced positive data for its phase I clinical trial in patients with advanced colorectal cancers.
The oncolytic viruses designed by Campadelli-Fiume express GM-CSF and the cytokine interleukin-12 (IL-12), which regulates T cell responses. “The immunostimulatory anti-tumour molecules accumulate in large amounts in the tumour bed and are absent from other compartments, where they would cause toxicity and side effects,” explains Campadelli-Fiume. In a recent study she showed a double-armed virus (R-123) was effective in tumour-bearing mice, with a 100% response rate achieved when given in combination with other immunotherapies (De Lucia M et al. Mol Ther Oncolytics, 2020).
So far, oncolytic viruses are largely being used in combination with other immunotherapies. “The idea is to use [oncolytic viruses] to deliver, locally, modalities that would… render the tumour sensitive to immunotherapy,” says Quéméneur. Cancer cells have developed immunosuppressive mechanisms and this explains why resistance builds up to some cancer drugs. For example in HER2-positive breast cancer, drug resistance develops in about 40% of patients. Campadelli-Fiume says what they can do with oncolytic viruses is “turn an immunologically cold tumour into an immune hot spot,” allowing current immunotherapies to succeed in patients where they may have previously failed. “The name of the game is combinations,” she adds.
Oncolytic viruses turn an immunologically cold tumour into an immune hot spot, allowing current immunotherapies to succeed where they may have previously failed
Match made in heaven
A particularly successful strategy so far has been combining oncolytic viruses with a drug that targets PD1/PD-L1 immune checkpoint proteins. Immune checkpoints are molecules on certain immune cells that control the intensity of normal immune responses, but are harnessed by cancer cells to prevent T cells from responding and killing cancer cells. Unfortunately, as Samson points out, “We’ve recently discovered that viruses quite strongly stimulate the upregulation of PD1 and PD-L1, and this limits the immune response against the cancer that’s stimulated by the virus.” Using checkpoint inhibitor drugs could prevent this by taking the brakes off any mounting immune response. “By combining a virus with PD1 or PD-L1 antagonist, we suddenly have a synergistic combination therapy… there’s a lot of ongoing work on combining viruses with PD1 and PD-L1 immune checkpoint inhibitors,” he says.
“Checkpoints [and oncolytic viruses] are a match made in heaven,” says Loskog, “because viruses will attract T cells and T cells are needed for checkpoint antibodies to work.” Following trials combining their oncolytic adenovirus, LOAd703, with conventional chemotherapy agents for pancreatic cancer (Musher BL et al. J Clin Oncol, 2020), Lokon Pharma are now collaborating to use their oncolytic virus in combination the PD-L1 inhibitor atezolizumab (Tecentriq) from Roche. They have initiated clinical trials in advanced pancreatic cancer, melanoma, and metastatic colorectal cancer. The virus is armed with two modifications − one to express the tumour-associated antigen CD40L, which Loskog says “kickstarts” immunity, and the other to express the receptor 4-1BBL, which “prolongs the response”.
Oncolytics Biotech in collaboration with SOLTI, a clinical cancer research cooperative (Spain and Portugal) have embarked on a clinical trial (AWARE-1) of the oncolytic reovirus pelareorep, with atezolizumab, in addition to other appropriate therapies, after successful results in metastatic breast cancer for combinations with systemic chemotherapy agents. The US biotech, Replimune, has also started trials with their herpes simplex oncolytic virus in combination with nivolumab (Opdivo), Bristol-Myers Squibb’s PD1 inhibitor. Their phase II trial in cutaneous squamous cell carcinoma and anti-PD1 refractory melanoma has shown a clear improvement on nivolumab alone. The company is recruiting for a further study to obtain regulatory approval.
Whether oncolytic viruses can be developed as monotherapies remains to be seen. Loskog says in the future she could see such viruses being used for small early-stage tumours, “but as soon as you have a little bit of disease spread, you get immunosuppression, and I do think you [then] need either chemotherapy or a checkpoint [inhibitor] or perhaps even both.” Oncolytic viruses could present an alternative for patients unable to tolerate anti-PD1 therapy. Replimune is currently running such a trial for treating cutaneous squamous cell carcinoma in people who have organ transplants.
Quéméneur says the next tranche of marketing approvals is likely to be for viruses in combination with other therapies, but this may not always be the case. Samson agrees: “There’s a possibility it could be used as a monotherapy, if we can engineer those other drugs into the virus, so that the virus expresses them adequately. And then you’ve got an all-encompassing combination treatment in a single virus.”
Tackling delivery
One other major issue concerns how these viruses should be delivered. The first generation of oncolytic viruses and those currently approved are given intra-tumourally. Lokon’s oncolytic virus therapy for pancreatic cancer is administered this way. “[Where] the tumour is located [inaccessibly], towards the back [of the pancreas], we do it endoscopically, [using] ultrasound guiding, and it works really well,” says Loskog. The approach allows a high number of viral particles to concentrate locally, although they will still activate systematic immunity through the lymphatic system. But Quéméneur says there can be problems: “Some tumours are very fibrotic, and just arriving with a needle in the tumour doesn’t mean that you [will] administer [the virus] everywhere in the tumour.” Plus, this approach is less viable where a patient has multiple tumours.
“Just arriving with a needle in the tumour doesn’t mean that you will administer the virus everywhere in the tumour”
Some trials are looking at ways to deliver oncolytic viruses intravenously (IV). “We believe that there is a lot of value in going IV,” says Quéméneur. A potential drawback, as Samson points out, is that “An intravenous route means that you get toxicity all over the body, whilst not delivering as much as you could to the tumour.” Together with Transgene, he has started a clinical trial to evaluate a compromise option by delivering an oncolytic virus, TG6002, via the hepatic artery − a targeted intravenous approach. “This is a local-regional delivery approach… where we are concentrating the virus at the bulk of the tumour in patients with liver-dominant colorectal cancer metastasis,” says Samson. The method is routinely used to deliver therapeutic agents into patients with liver tumours. Quéméneur suggests in future the delivery route is likely to depend on the type of tumour: “We know that some are poorly vascularised [and others] pretty well vascularised.’
Safety is of course another important issue. To date oncolytic viruses have been found to be relatively safe, compared to other cancer treatments. In clinical trials, in addition to local inflammation at the injection site, around 30% of people treated with T-Vec experienced flu-like symptoms; 2% of people had severe reactions, mainly cellulitis (EMA Imlygic Product Information: Annex 1, retrieved 16 December 2020). “You can have cytokine release syndrome a few hours after injection,” says Loskog, but “usually they are rather mild… nothing has happened that we feel is really dangerous.”
Samson says that while viruses give an acute toxicity − “as you can imagine, dumping a whole bunch of virus into your bloodstream will make you feel unwell until the body deals with it,” there are no long-lasting effects, “which makes them quite attractive as a combination therapy.” Transgene’s viruses show a similar safety profile, says Quéméneur: “In our trials we have never seen any kind of cytokine storm as strong as was reported for CAR-T or other antibodies. So I think that it’s a more tolerable therapy than other existing immunotherapies.”
“There are no long-lasting effects with oncolytic viruses, which makes them quite attractive as a combination therapy”
Who benefits?
There is real excitement around the potential of oncolytic viruses, but they do not work for all patients and part of current research efforts is to discover which patients will benefit. “We really need a couple of big breakthroughs with viruses, making a big difference to patient outcomes, and once we have those, we can start to pick out who responds better, who responds less well,” says Samson.
One signifier is tumour burden says Loskog, with higher tumour loads creating more immunosuppression, “but otherwise, it’s very difficult to predict who will respond. I have seen patients with higher tumour load also respond, and someone with a rather small tumour not respond. So I don’t think we fully understand it.” Lokon are now screening for biomarkers to try to ‘fish out’ what’s going on. Transgene are also looking for clues: “We don’t have a clear vision of the mutation profile or kind of phenotype that would be associated with a good prognosis, but we have some ideas, and [are carrying out] some sampling and genotyping studies.”
It is likely to be a few years until the bulk of current research comes to fruition and many of the oncolytic viruses being developed receive marketing approval. “I think that within a five-year period we will definitely have more approved viruses, and within a 10-year period, it will be one of the options for several different tumour types… likely combined with checkpoint [inhibitors],” says Loskog.
For Quéméneur, oncolytic viruses represent an important new tool in weaponising the human immune system to fight cancer. It is the ability to rationally engineer viruses that can deliver any number of immunotherapies that will ultimately provide the significant therapeutic impact. “We want to keep the oncolytic properties of the virus, [but] we really want to use them as advanced nano-machines to control immune profiles… I think we are moving from a vision where viruses would be used mostly for their oncolytic properties to an era where they will be used as drug delivery systems,’ he concludes.
Illustration by Sara Corsi